The nursing associate role was created to address a skills gap and meet workforce needs. This article describes a table-top simulation designed to help embed the role in existing teams.
Abstract
The nursing associate role was created to bridge the gap between healthcare support workers and registered nurses, and formalised by the Nursing and Midwifery Council in 2018. Embedding the role into the clinical setting requires a comprehensive understanding of the scope of practice and benefits to the nursing workforce. This article discusses the use of workforce redesign and tabletop simulation to engage and develop local understanding and ownership in inpatient wards. This approach fostered the senior nursing support needed to embed the nursing associate role in a financially viable model, and gave nurses a much greater understanding of the role and how it would fit in their clinical teams.
Citation: Cox S (2021) Using workforce transformation to embed the nursing associate role. Nursing Times [online]; 117: 9, 32-34.
Author: Sue Cox is head of nursing for workforce transformation and education, Guy’s and St Thomas’ NHS Foundation Trust.
- This article has been double-blind peer reviewed
- Scroll down to read the article or download a print-friendly PDF here (if the PDF fails to fully download please try again using a different browser)
Introduction
The Shape of Caring review (Willis, 2015) was commissioned by Health Education England to review the education and training of registered nurses (RNs) and care staff providing care for complex patients. It identified a gap in skills and knowledge between healthcare assistants and RNs. To bridge this gap, the nursing associate (NA) role was created and became regulated by the Nursing and Midwifery Council (NMC) in 2018. The NA role was designed to:
- Free nurses time so they can deliver more complex care;
- Provide a progression route into graduate nursing;
- Create a career development and progression pathway for support staff.
The Interim NHS People Plan (NHS, 2019) promoted the NA role as a way to increase access into nursing. This article explores how a large acute and community trust used workforce transformation to implement the NA role alongside the development of RNs to meet the Nursing and Midwifery Council’s (2018) standards for future nurses.
The trust has worked hard over the years to match NMC requirements to the needs of the patient population and has a robust approach in line with the standards and expectations for safe staffing set out by the National Quality Board (NQB, 2016). Despite year-on-year growth and having more nursing staff in post, the trust’s vacancy rate remained static at 12-14%. It was acknowledged that a different way of working was needed to meet the growing needs of our patient population and to redesign our nursing workforce.
In January 2020, there were 123 apprentice NA posts across five clinical areas in the trust. The posts are being rolled out, directorate by directorate, to ensure they are embedded and the role is valued. However, large-scale change was needed to support increasing patient activity and acuity, so a five -year workforce plan was created.
Five-year workforce plan
Each directorate completed a programme of workforce redesign and review as part of the annual establishment review. The safer nursing care tool created by the Shelford Group and endorsed by the National Institute for Health and Care Excellence (2014) was used to guide staffing numbers. It is important that this tool is used alongside professional judgement, patient acuity and service activity plans, to support the decision-making process.
The review used future shift analysis at set timeframes (2019, 2021 and 2024) to map the day-to-day establishment required in five years’ time, predicting the number of different band nurses and support workers required on each shift (Table 1).
The aim of future shift analysis was to embed the NA role in the nursing team with the support of senior nurses, while meeting the required skill mix for the patient population. We made it clear that this was not about decreasing the number of RNs, but about embedding the NA role and providing senior nurse leadership.

The workforce plan predictions included an increase in band 6 requirements, a change in band 3 and 5 requirements and the addition of the NA role, where appropriate and safe. Consideration of budget and financial constraints were key to ensure this was cost neutral or reflected acuity and activity changes.
The resulting five-year workforce plan rebuilt the nursing establishments to make them fit for purpose and incorporated the NA role, matching patient acuity and ensuring the right staff, with the right skills, at the right time.
Once it had been agreed that it was appropriate for the NA role to be part of the nursing establishment, sufficient numbers of NAs were needed in each establishment to deliver and maintain a consistent workforce model. This helps to support greater understanding and use of the role, and improves the experience of all staff and patients involved.
Following a review of all directorates’ five-year workforce plans, a template establishment was created for a typical 28-bedded ward using the team nursing approach and incorporating the new NA role. This template guided clinical teams on how the new role could be embedded in clinical areas, while being mindful of the need for variation, depending on the size of ward and patient acuity.
Tabletop simulation
Tabletop simulation (Box 1) was chosen to support the directorates in testing these new establishments and embedding the NA role in their clinical teams. Simulation allows nurses to practise clinical and decision-making skills and challenge underlying assumptions through real-life situational experiences, without compromising patient care (Kim et al, 2016).
Box 1. Tabletop simulation: how it works
- The clinical setting is designed using a ‘bird’s eye view’, reflecting the layout of the setting undergoing simulation to create a sense of reality
- The multidisciplinary team are represented by figurines that move about the clinical area and have a patient allocation that represents a typical day and patient caseload
- A typical shift will be run through in ‘fast time’, including the usual handovers, rounds and meetings
- All attendees have a handover sheet and allocate their shift team
- Figurines representing staff are moved around the setting like chess pieces
- The shift includes scenarios that are common to the clinical area
- The shift starts and the team decides which staff member provides which aspect of care/ward task in their team
- Additional scenarios and tasks can come in at any point in the day
- A clock is placed under staff who are unavailable, and removed when their task is complete
- At any point in the scenario, “time out” be can called if there is a wish to discuss a decision taken. The scenario can be replayed after the discussion
Tabletop simulation has been used to support directorates to test and confirm future establishments through skill-mix optimisation and re-profiling how each team member works. The aims and objectives of the tabletop simulation are to:
- Practise workforce transformation and new establishment setting in a safe environment;
- Challenge current practices and ways of working;
- Test and reinforce decisions for future ways of working;
- Support planning for the next steps of workforce transformation;
- Enable the current workforce to design and lead the change, enhancing engagement and ownership;
- Increase understanding of the NA role.
How it works
The simulated shift is followed by a debriefing session, using an approach such as the Plus/Delta model. This is a simple model that does not need a trained debriefer; it allows participants to identify what went well (plus) and what could be done differently (delta), thereby helping individuals to learn how they can work better as part of a team (Gardener, 2013). This debriefing method was also used during ‘time outs’ or pauses throughout the simulation activity to explore the rationale behind actions or decisions.
Evaluation
Ten simulation sessions have taken place to date, involving 31 different ward settings and 90 participants. For the purpose of the sessions, the directorates grouped together staff from three to six wards with similarities in layout and patient speciality.
Two wards completed individual sessions due to their different patient populations. Each session had an average of nine participants (range: three to 14 per session) and included nursing assistants, staff nurses, ward managers, matrons and heads of nursing.
Questionnaires were completed before and after the tabletop sessions to evaluate how they increased understanding. The pre-session survey revealed that individuals felt unsure of the NA role and how it would fit into the team. Participants were also nervous and unsure about how the session would work and any associated benefits. Before the session, 53% of participants reported not knowing the benefits of the NA role; afterwards, that fell to 13%.
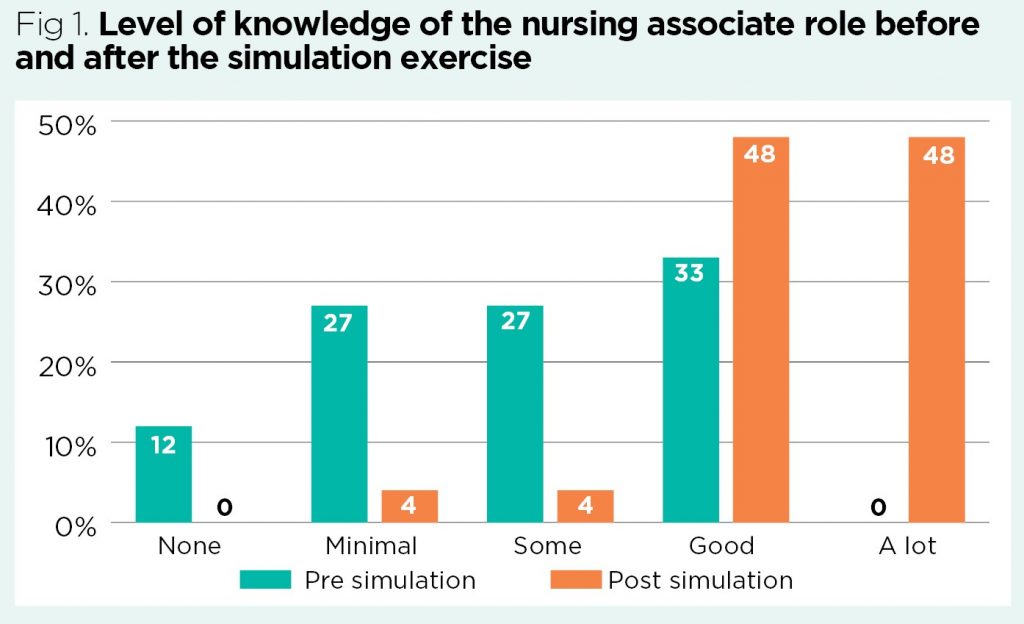
Staff were impressed with the engagement and interest from the team. It gave individuals a good understanding of the NA role and scope of practice (Fig 1), and enhanced team working, as well as an understanding of how the role would fit into the nursing establishment.
Preparing the workforce
Active, meaningful engagement and collaboration is vital for the successful introduction of any role in a team. An overview of the understanding of the NA role across the organisation was essential and gained through wide-scale nursing and midwifery staff surveys and informal interviews with the apprentice NAs. The intelligence gained informed the communication strategy, highlighting areas of focus, both in knowledge deficit and particular clinical areas.
Workshops on designing the nursing workforce for the future were held for all nursing staff. The aim was to improve engagement and codesign role definitions for band 2 to band 7, incorporating the future-nurse standards of proficiency for RNs (NMC, 2018) and the NA role.
While the directorates were completing the tabletop simulation sessions, promotional events took place across the trust with information about the nursing associate role. This included apprentice NA advocates, case studies and a quiz on the NA scope of practice, which provided a ‘jumping off’ point to help further discussion. As attendance at the promotional events varied, a ‘one-stop’ NA trolley was designed to travel the wards, providing this information to those unable to leave the clinical environment.
Future plans
The aim is for all directorates to complete one tabletop simulation to test and support establishment setting in inpatient, ambulatory and community settings. New virtual and socially distanced formats of the tabletop simulation are being designed so the tool can continue to be used.
To maximise the benefits of the table-top simulation and engage with wider clinical teams, a ‘train the trainer’ package is also being created. This will enable directorates to lead and complete the simulation sessions in all their clinical areas as required; multidisciplinary teams will be involved to help with workforce and service redesign.
Conclusion
This approach established that creating a clear vision and developing plans driven by local ownership and engagement strongly supports workforce redesign. Large-scale introduction and a clear communication strategy supports the successful implementation of new roles such as that of the NA. Staff feedback from the tabletop simulation suggests an increased understanding of this role, its benefit and place in the nursing establishment.
Ongoing development of the communication strategy and additional tabletop simulation sessions are being planned to support the widespread use of the workforce transformation tools across all clinical settings.
Key points
- The nursing associate role was created to address a skills gap found in a review of education and training for registered nurses and care workers
- Completing a five-year workforce plan helped clinical teams to engage with embedding the nursing associate role
- Tabletop simulation was used to test the workforce transformation plan
- A clear, inclusive and comprehensive engagement and communication strategy is needed to successfully introduce new roles
- Redesigned tabletop simulation is now being used for further roll-out across inpatient, ambulatory and community settings
- Acknowledgement
I would like to thank Katherine Milner, deputy head of nursing for workforce transformation and the workforce team for their support with this programme of work.
I would like to thank Professor Lisa Bayliss-Pratt, pro-vice-chancellor, Faculty of Health and Life Sciences at Coventry University and the Florence Nightingale Foundation for the opportunities and support provided during the Aspiring Director of Nursing Course.
Gardner R (2013) Introduction to debriefing. Seminars in Perinatology; 37: 166 –174.
Kim J et al (2016) Effectiveness of simulation-based nursing education depending on fidelity: a meta-analysis. BMC Medical Education; 16: 152.
National Institute for Health and Care Excellence (2014) Safe Staffing for Nursing in Adult Inpatient Wards in Acute Hospitals. NICE.
National Quality Board (2016) Supporting NHS Providers to Deliver the Right Staff, with the Right Skills, in the Right Place at the Right Time: Safe Sustainable and Productive Staffing. NQB.
NHS (2019) Interim NHS People Plan. NHS.
Nursing & Midwifery Council (2018) Future Nurse: Standards of Proficiency for Registered Nurses. NMC.
Willis G (2015) Raising the Bar. Shape of Caring: A Review of the Future Education and Training of Registered Nurses and Care Assistants. Health Education England.
 Nursing Times Resources for the nursing profession
Nursing Times Resources for the nursing profession 

Have your say
or a new account to join the discussion.